Abstract
Introduction: The genomic heterogeneity in Acute Myeloid Leukemia (AML) has been shown to affect the overall prognosis and should be taken into account to decide the best course of treatment. Study of AML genomic landscape by The Cancer Genome Atlas (TCGA) research network by Ley, et.al, analyzed the genomes of 200 patients (pts) with de-novo AML and showed at least one potential driver mutation in nearly all AML samples and further classified these mutation in 9 functional categories: Myeloid transcription factor and fusion genes, Tumor suppressor genes, gene encoding Nucleophosmin, Activated signaling genes, DNA methylation related genes, Chromatin modifying genes, Cohesion complex genes and Spliceosome complex genes . The availability of Next Generation Sequencing (NGS) has allowed easy characterization of patient samples. However, this has now became increasingly important to prioritize the influence of different mutations clones so as to give actionable and prognostic information. We developed an Integer Weighted Genomic Mutation Score (GMS) to address this in the context of the TCGA data and applied this to a retrospective cohort of pts with AML. The goal was to meaningfully stratify the Intermediate risk AML patients per current ELN criteria based identified by NGS technique into low and high risk group and correlate this with clinical outcome.
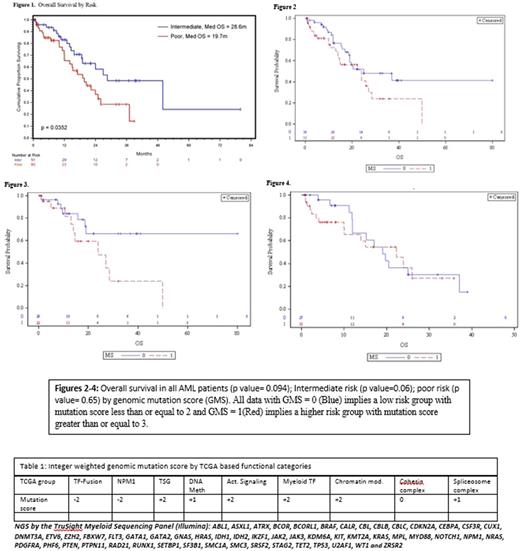
Study Method: We screened 1200 AML patients at our institution from 2010 to 2016 and identified 111 patients from our hospital database who had information on both cytogenetics and gene mutation detected by NGS. We queried for the diagnosis of AML and demographics, Cy, NGS and OS. We divided the patients into 3 groups according to their cytogenetic risks- Favorable (FCy), Intermediate (ICy),Poor (PCy). Mutations in 54 genes associated with myeloid disorders were tested in NGS by using the TruSight Myeloid Sequencing Panel (Illumina) (Table1). We also performed flow cytometric evaluation on a BD FACSCantos™ II 3-laser (405, 488, 630 nm excitation sources), 8-color flow cytometer (BD Biosciences, San Jose, CA, USA) and data analyzed using BD FACSDiva software. We then utilized the TCGA data by Leyet.al and developed a system of Integer Weights forthe Genomic Mutation Score (GMS) obtained by targeted NGS at Houston Methodist Hospital mentioned below. GMS was designed by assigning a score for each genomic mutation between the range of negative 2 (-2) for good risk to positive 2 (+2) for each of 9 TCGA mutation categories .The total IWGMS for each patient was calculated by the sum of mutation scores in each 9 categories. A score of 3 or greater than 3 was defined as high risk. We then performed a retrospective analysis of 111 AML patients to correlate the GMS with 2 year mortality and survival outcome. Statistical Analysis was done using multivariate logistic regression method.
Results: Pts were grouped into 51 intermediate risk and 60 poor risk cytogenetics. Median age of the pts was 66 years and 57.6% were male. Immunophenotyping of CD34 and CD38, and CD117 did not emerge as significant predictors of survival when adjusting for covariates. 32% of patients underwent allogeneic stem cell transplant as consolidation therapy. Median overall survival for the entire study population was 24 months with a median follow up time was 20.01 months (95% CI; 15.77 - 25.17). Univariate analysis using cox proportional hazard method showed age and cytogenetics risk as a statistically significant predictor of overall survival as shown in Fig: 1. Overall survival in all AML patients and Intermediate risk patients showed a trend toward better OS with lower GMS but no such trend was seen in poor risk AML patients as shown in Fig: 2-4.
Conclusion: We have developed an GMS system to further stratify Intermediate Risk AML patients into high and low risk groups. Age and cytogenetics risk per ELN criteria were independent prognostic factor for overall survival in our study cohort as expected. Patients with lower GMS in our study cohort had a trend towards better OS but patients with high GMS had a trend towards worse OS in intermediate risk AML patients. Larger size prospective study is required to validate this scoring system; it has a great potential to identify high risk patients among Intermediate risk group and plan different consolidation therapies to further improve their outcomes.Further treatment related analysis will be presented at ASH,Atlanta 2017.
Iyer: Takeda: Research Funding; Genentech: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal